- Home
- osteoarthritis
osteoarthritis

Osteoarthritis (OA) effects over 8 million people in the UK.
The most common joints affected are:
- Knee
- Hip
- Cervical Spine (neck)
- Lumbar spine (lower back)
- Shoulder
- Ankle
- Wrist
- Big toe
- Fingers
Onset is most common after the age of 40 and becomes more common as we age.
Contrary to popular belief, OA is not a wear and tear disease. In the vast majority of cases, it causes is completely genetic. The exception being, if you are unfortunate enough to fracture or badly sprain the ligaments of a joint, you may be more likely to suffer OA in that particular joint as a result, due to damage caused to the outer surface of the bone.
Actually calling OA a ‘wear and tear’ condition can be very unhelpful as it leads people to presume that the more they move, the more ‘wear and tear’ they will cause. If you read on you will find the exact opposite is true….
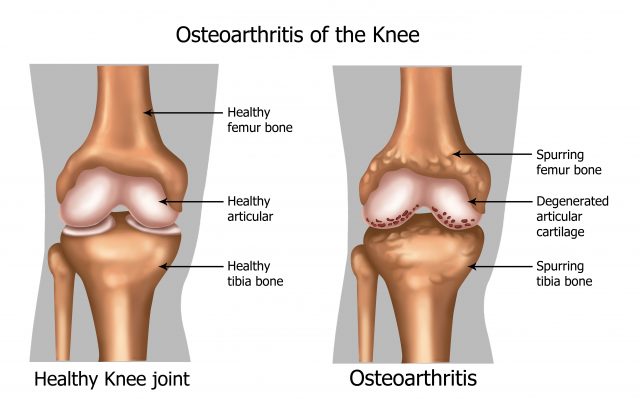
What actually happens to the joint?
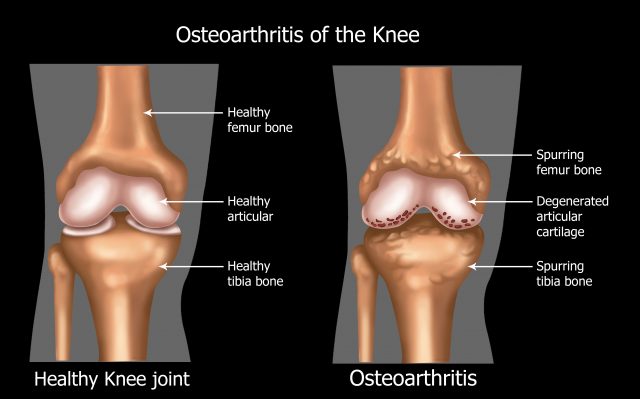
A joint is where two bones meet. The image above shows a knee joint where the thigh bone and shin bone articulate. In an arthritic joint, the articular cartilage that protects the outer surface of the bones becomes thin and can eventually erode away. This exposes the sensory nerve endings and can cause pain. The knee is also a ‘synovial joint’ which means that synovial fluid is secreted into and around the joint surfaces. Synovial fluid helps to nourish and protect the joint and also acts as a lubricator, like WD40 for your body. However synovial fluid is only secreted into the joint when we move, not when we’re static, Many joints in the body are synovial joints and therefore feel much better with regular movement.
What are the symptoms of OA?
Pain:
Arthritic pain can be constant or intermittent pain accompanied by a feeling of stiffness and loss of joint mobility.
Pain can be: a dull ache, throbbing or a sharp pain
The pain can often be accompanied by swelling but not always.
Where will the pain be felt?
The most common area to feel pain is on the particular joint itself but patients will often report referred pain which is simply pain that travels away from the joint. For example, patients with hip OA often feel pain in the thigh and sometimes as far away as the knee.
Aggravating activities can include :
Prolonged static postures (sitting/standing/lying), cold temperatures.
Easing activities can include:
Regular changes in posture, movement, and exercise, stretching, joint support, warm temperatures and application of heat to the area.
Pain pattern:
The joint will often be stiff and painful first thing in the morning, ease once you get up and move that particular joint. The symptoms will tend to depend on what activities are performed through the day (immobility and prolonged static postures usually worsen symptoms). At night sleep can often be disturbed after lying in the same position for too long which causes increased stiffness and pain.
What is the best way to treat and manage OA?
Exercise, exercise, and more exercise! The scientific evidence supports the use of stretching and strengthening exercise in the management of OA. It is important to maintain the range of movement and muscle strength around the joint to enable optimum function as we know stiff and or weak joints are more painful. For load bearing joints such as the knee and hip, non-weight bearing exercise such as swimming and cycling are particularly helpful.
At Newcastle Physiotherapy we also strongly support the use of manual therapy in conjunction with a progressive exercise program. Specific soft tissue mobilization and massage techniques help to maintain muscle balance. Joint mobilization techniques help to stretch the articular tissues around the joint, such as the joint capsule and the supporting ligaments. Passive stretching and a technique called proprioceptive neuromuscular facilitation help to maintain and improve joint and soft tissue mobility, Neurodynamic exercises help to improve the mobility of the central nervous system and peripheral nerves.
If the pain is limiting the progress of your exercise program we often use acupuncture and dry needling techniques to provide pain relief. Other treatment techniques and modalities which can help with pain management include:
- Supportive Taping
- Prescription of joint supports
- Fitting of custom orthotics (insoles)
- Prescription of transcutaneous electrical nerve stimulation (TENS)
- Advice on the use of appropriate medication and joint health supplements
- Referral for ultrasound-guided corticosteroid (pain-killing drug) injections with our own specialist physiotherapist and radiologist.
